Accessing Affordable Care: How Much Is Health Insurance in Arizona?
Explore Arizona health coverage statistics and medical assistance topics and get insurance questions answered

Healthcare leaders across the U.S. are grappling with managing rising healthcare expenses while also making care more accessible and affordable for patients. One major factor in access to care is whether an individual has health insurance, which is influenced by the cost of insurance in their state.
In Arizona, the average monthly cost of health insurance for 2022 is $577, and the average yearly cost is $6,924. However, individual health insurance costs vary depending on location, income, and other factors.
An investigation into how much health insurance in Arizona costs must begin with an examination of what’s happening nationwide and the factors that impede access to care for some U.S. residents, including rising healthcare costs. According to Centers for Medicare & Medicaid Services (CMS) data interpreted by the Peterson-KFF Health System Tracker:
- Since the 1970s, healthcare and health insurance costs have been rising across the U.S. Health spending went from just over $74 billion in 1970 to $1.4 trillion in 2000, and more than doubled by 2019 ($3.8 trillion).
- Healthcare costs per person are projected to rise from $11,582 in 2019 to an estimated $18,000 by 2028.
Access to healthcare is important
Access to quality, affordable healthcare services is essential to improving health outcomes and reducing health disparities. Factors that limit access to care include lack of health insurance, lack of access to transportation, and limited healthcare resources in rural and low-income communities.
One of the major barriers to achieving equitable access to care in the U.S. is the high cost of care. Healthcare spending in the U.S. is nearly double the average for member countries in the Organization for Economic Cooperation and Development (OECD), according to a report on healthcare spending published in JAMA.
Why do healthcare costs keep rising in the U.S.? Reviewing U.S. healthcare from a global perspective, the Commonwealth Fund attributes cost increases to the higher prevalence of chronic disease and obesity; lower supply of physicians; and higher use of costly technologies, including MRIs and procedures such as hip replacements.
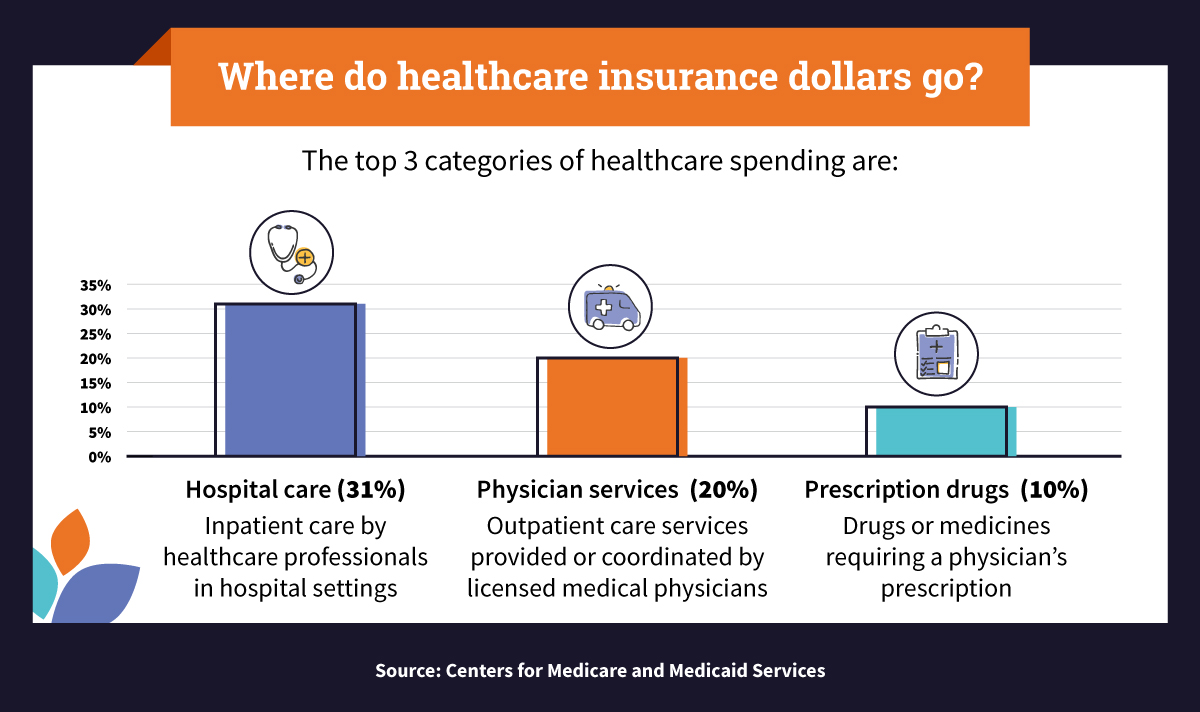
According to 2019 data from the CMS, hospital care, physician services, and prescription drugs were the largest categories of healthcare spending. The top 10 categories of national healthcare expenditures were:
- Hospital care (31% of all spending): This includes intensive care units (ICUs), where seriously ill patients at risk of dying are treated, and non-ICUs, where patients receive care (sometimes urgent care) such as treatment of minor cuts, burns, sprains, and throat infections.
- Physician services (20% of all spending): These services are provided by a licensed physician in various healthcare settings, but not offered while admitted in the hospital. Physician services are focused on health promotion, disease prevention and management, patient education, and diagnosis and treatment of acute and chronic illness.
- Prescription drugs (10% of all spending): This category includes prescription medications, including opioids, depressants, and stimulants. Many prescription drugs can lead to misuse, overdose, and side effects; for this reason, a prescription is required from a licensed physician or a nurse practitioner.
- Other personal healthcare costs (5% of all spending): This category includes costs for ambulance services and care provided in nontraditional settings, including community centers, schools, and workplaces.
- Nursing care facility services (5% of all spending): This includes a wide range of health and personal care services delivered by nurses in residential facilities, assisted living facilities, and nursing homes.
- Dental services (4% of all spending): This category describes a wide range of services that dentists in offices and various healthcare facilities provide.
- Home healthcare services (3% of all spending): From wound care to monitoring of serious illness, these services are provided in an individual’s home by licensed medical professionals.
- Other professional services (3% of all spending): These services are provided by professionals such as chiropractors, podiatrists, and occupational therapists.
- Other nondurable medical products (2% of all spending): These products include medical equipment, such as disposable gloves, rubber or plastic hose used for catheters, and syringes.
- Durable medical equipment (2% of all spending): This category includes durable medical equipment used to provide therapeutic benefits to a patient for certain medical conditions.
Ethics and economics of universal access to healthcare
In the U.S., the right to care and the government’s role in providing access to healthcare are contentious topics debated at the highest levels. Wherever an individual is on the political spectrum, it can be agreed that health is foundational for pursuing opportunities in life. A healthy individual can build a family and go to work.
While some believe that it’s ethical to help all individuals gain access to care, regardless of their socioeconomic background, others are concerned about how much that approach would cost. On one side of the political spectrum are people who believe that the millions of uninsured are being denied their basic right to healthcare and that the government should ensure basic access to healthcare to every American. On the other side of the political spectrum are people who believe that making healthcare an essential government service would lead to increased taxes, a more powerful central government, and a loss of individual choice.
However the issue is viewed, cost is a big component of access to healthcare. Some people have the financial means to pay for their own healthcare. Others receive healthcare benefits from their employers. Others can benefit from government programs, such as Medicare and Medicaid. Access to healthcare for all remains elusive. Other values important in healthcare include equitable access, affordable access, quality, and choice.
Here are some statistics:
- According to U.S. Census data, 8.6% of people in the U.S. (28 million) didn’t have health insurance coverage during 2020, up from 8% (26 million people) in 2019.
- At full strength throughout much of 2020, the COVID-19 pandemic has translated into people dying from lack of healthcare. According to Families USA, for every three COVID-19 deaths nationally, about one can be linked to health insurance gaps.
The state of Arizona has mirrored what’s happening nationally in regards to patient access to care. For example:
- There were 60,000 more uninsured Arizonans in 2019 compared to 2018.
- In Arizona, there were 99,954 COVID-19 infections and 2,013 deaths linked to health insurance gaps from January 22, 2020, to August 31, 2020, according to data from Families USA.
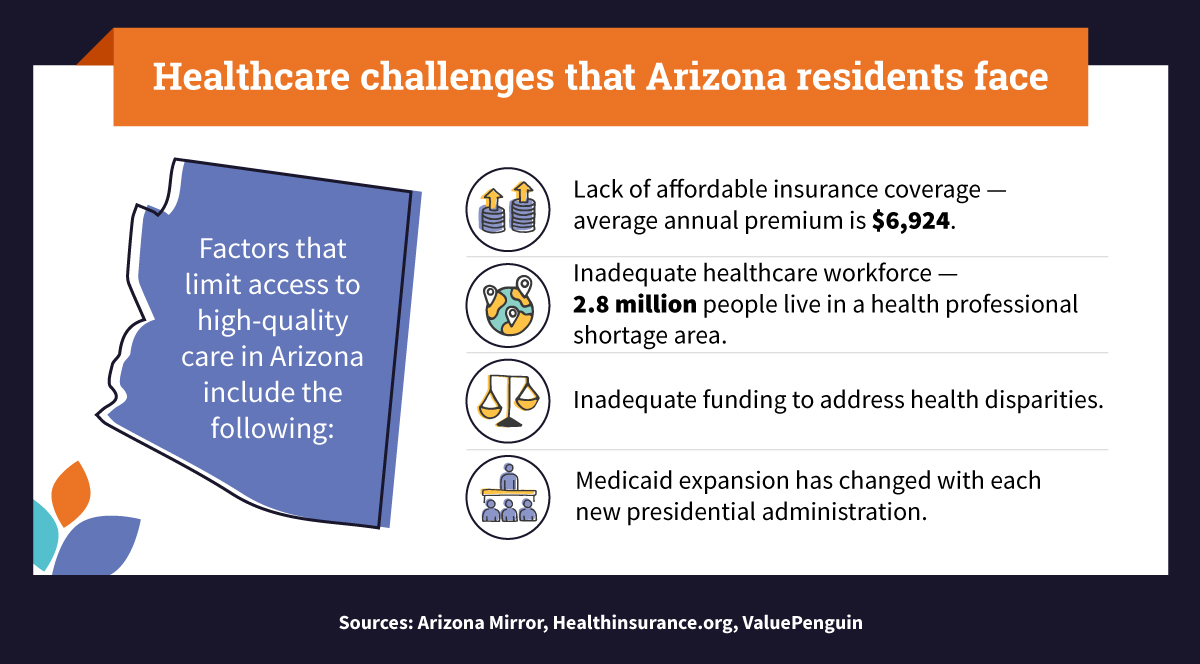
The following data reveals some of the factors limiting healthcare access in Arizona:
Arizona health coverage statistics
According to census data, the uninsured rate in Arizona decreased between 2010 and 2017: In 2010, 16.9% of Arizona residents were uninsured; in 2017, the rate fell to 10.1%. This success in improving coverage was short-lived. The rate rose again in 2018 and 2019 (to 10.6% and 11.3%, respectively).
Why do challenges in health coverage in Arizona persist? Barriers to access in Arizona include the following, according to Vitalyst Health Foundation:
Insurance affordability
Despite the gains made under the Affordable Care Act (ACA), many in Arizona lack the financial stability to access quality healthcare. In 2018, about 734,000 nonelderly Arizonans (aged 0 to 64) were uninsured, according to state healthcare data from KFF. This uninsured rate was higher than the national average.
Older adults (aged 50 to 64) are among those most affected by coverage gaps. AARP highlights some key statistics about Arizona’s health coverage affordability gap. Here are some statistics about older adults in Arizona who aren’t enrolled in a group plan:
- Over 64% of older adults in Arizona pay high premiums and out-of-pocket costs, making coverage unaffordable.
- About 46% don’t receive financial help with healthcare coverage costs.
- 14.2% delayed medical care due to high costs.
Adequate healthcare workforce
In Arizona, 40% of people live in healthcare shortage areas. Areas and population groups with a shortage of health professionals — primary medical, dental, and mental health — are designated as health professional shortage areas (HPSAs). This means that the healthcare workforce is inadequate to meet community needs. According to data from KFF, Arizona ranked No. 9 in total HPSA designations (236) as of September 2021. The state requires 653 new practitioners to remove an HPSA designation.
The workforce also faces government and insurance industry regulations that can increase costs and reduce efficiency, according to the American Medical Association (AMA). An insurance industry regulation known as prior authorization describes a process to determine whether insurance will cover a prescribed product or service. This can also include the use of medical equipment. The time to get prior authorization adds to the problem of an inadequate healthcare workforce by reducing the efficiency of a workforce already stretched to the limit. This can minimize the effect on patient care while increasing expenses. The AMA reports that addressing physician shortages is key to improving access to healthcare.
Health disparities
Barriers to access to healthcare in Arizona can lead to health disparities. Inadequate funding or investment to address the social determinants of health can create a chain reaction leading to health disparities. For example, lack of health insurance puts people at risk of not being able to afford care when an illness or accident comes unexpectedly. Additionally, preventive healthcare can help prevent illnesses, surgeries, and hospitalizations, but without a way to pay for it, many people delay care, adding cost burdens on the entire health system.
The Arizona Department of Health Services has launched campaigns to improve access to healthcare to underserved communities. For example, interpretive services, resources for language learning, and additional information are available to help populations with limited English proficiency (LEP) access the health services they need. Additional strategies for mitigating health disparities include stabilizing the individual healthcare insurance marketplace, ensuring adequate funding of children’s insurance programs, retaining Medicaid expansion, and implementing expansion across other U.S. states.
Requirements changes
With presidential administrations changing and focusing on different political priorities, healthcare policy ideas evolve. Consider Medicaid expansion, a provision of the ACA calling for extending Medicaid eligibility to cover more low-income Americans.
The Trump administration wanted people to have to work to qualify for Medicaid, and it approved Arizona’s 2020 proposed work requirement, which would have led to some unemployed people missing out on access to healthcare benefits. However, amid legal uncertainty, the requirement was never implemented. The Biden administration then withdrew approval in 2021, eliminating the work requirement.
The Center on Budget and Policy Priorities (CBPP) reports that in 2019, 2.2 million uninsured adults lived in states that didn’t adopt the Medicaid expansion component of the ACA, meaning that even those below the poverty line were required to pay for healthcare coverage on their own. One of the aims of Medicaid expansion is to reduce racial disparities and improve access for individuals who don’t have a pathway to affordable coverage.
Answers to all your Arizona insurance questions
The answers to the following common health insurance questions can help Arizonans learn about and access healthcare benefits:
How much does health insurance cost in Arizona?
Health insurance rates in Arizona vary by region, but the average statewide monthly premium for 2022 is $577, with an average annual premium of $6,924. To learn about the rates for different regions, individuals can search HealthCare.gov using their postal code.
For example, a search for 85364 (Yuma County) reveals that the average premium for a bronze plan is $529. The bronze plan, one of four categories in the Health Insurance Marketplace, offers individuals with the lowest monthly premiums but higher costs to receive care. In 85530 (Graham County), the average premium for a bronze plan is $425.
What are the Arizona medical assistance programs?
Arizona medical assistance programs include offerings and resources from the Arizona Health Care Cost Containment System (AHCCCS) — the state’s Medicaid agency — and other organizations.
- Arizona Health Care Cost Containment System: Information from the AHCCCS about low-cost healthcare options for qualified individuals and families.
- Arizona Department of Insurance and Financial Institutions: Information on consumer tools, insurance, and insurance companies that serve Arizonans.
- Arizona Health Matters: Data on the Arizona population and community health information for individuals, planners, and policymakers.
- Arizona Alliance for Community Health Centers: Information about health center programs that serve communities and disadvantaged populations.
- Cover Arizona: Information about the types of healthcare coverage available, plans, and prices, as well as where to find in-person help.
- Medicare Rights Center: Information about access to affordable health care for older adults and people with disabilities.
- Arizona State Health Insurance Assistance Program: Information for older adults about Medicare assistance, including where to find local offices.
- Healthinsurance.org, Arizona: Comprehensive guides to individual and family health coverage.
- HealthCare.gov: The federal government’s health insurance exchange site.
How do I apply for medical assistance in Arizona?
Arizona has expanded Medicaid coverage to include adults with incomes that are characterized as low or very low. A one-person household with a maximum annual income of $17,131 is considered low income and qualifies for the Arizona Medicaid medical assistance program, according to Benefits.gov. For a four-person household, the maximum annual income can’t exceed $35,245.
Medicaid Assistance
In addition to the income qualification for Medicaid assistance, an individual must be a resident of Arizona and a U.S. national citizen, permanent resident, or “legal alien.” Assistance is also available for pregnant individuals.
Qualified residents of Arizona can apply for medical assistance on AHCCCS’ Health-e-Arizona Plus online application portal (along with nutritional and financial assistance). When applying for medical assistance, individuals need to present key pieces of information, including the following:
- Identification that proves citizenship, or green cards, if a non-U.S. citizen.
- Social Security number or proof of having applied for one.
- Birth certificate for every applicant.
- Contact information of a landlord or neighbor, including address and phone number.
- Statement from a nonrelative who does not live with the applicant that verifies the applicant’s address.
- Proof of all household income including money sources from the current month and previous month.
- Documentation that proves that employment has ended (with last date paid) for individuals who lost their jobs.
- Verification of medical insurance other than from the AHCCCS.
Hospitalized applicants can expect a decision within seven days of the application date. Those who are pregnant are typically notified within 20 days. Other applicants should learn about a decision no more than 45 days from the application date. Applicants who are denied assistance can request an appeal. Information about the appeals process can be found on the Arizona Department of Economic Security website.
Successful applicants can expect an approval letter. If eligibility can’t be determined due to missing information, applicants will receive a Request for Information letter. The information requested can be shared via Health-e-Arizona Plus.
Other Assistance Programs
Individuals who don’t qualify for Medicaid assistance may qualify for reduced-cost insurance on the Health Insurance Marketplace through premium tax credits. Enrollees can explore cost savings options via the HealthCare.gov site.
Individuals can also gain access to affordable medical services and insurance advice by contacting their local community health center.
Improving access to care in Arizona
What’s the future of Arizona healthcare? Budget considerations in the aftermath of COVID-19 seem to be on the top of the agenda, according to the State of Reform, a political advocacy organization focused on bridging gaps between healthcare and health policy. Additional important topics in Arizona’s healthcare landscape include managing an increase in Medicaid applications and providing culturally sensitive medical care to communities.
Local organizations and healthcare providers can help address these issues and improve access to sufficient care in their communities by providing quality medical assistance information and resources. Leaders of healthcare organizations have important roles to play in strengthening patient access to care and reducing healthcare disparities as they shape the policies of their organizations.
For individuals, finding information on how to access insurance and assistance programs can be daunting. In Arizona, one of the first steps is to determine if you qualify for assistance. Your income, place of residence, and other factors all matter in determining whether you qualify for healthcare and insurance assistance. Reaching out to local healthcare organizations for support can be an essential step. Improved access to care, insurance, and assistance programs are key to enhancing the wellbeing of individual communities in Arizona.
Infographic Sources:

Knowledge and skills for healthcare management careers
At the manager and executive level, healthcare management careers usually require either a master’s degree or a doctorate. Professionals at this level are responsible for managing people and operations, and will be tasked with innovating and setting strategy according to an organization’s goals.
Effective management in any industry requires a wide range of experience, both technical and interpersonal. In the healthcare industry, managers and administrators must not only have experience in healthcare — whether that comes from a clinical, research, insurance, or related background — they must also have a solid foundation in business concepts, such as accounting, marketing, operations, or human resources. In addition, they need the interpersonal skills that enable them to be effective administrators or managers.
The skills and experience required for an effective career in healthcare management include:
Healthcare industry knowledge
Healthcare is a highly complex, heavily regulated industry. To be an effective leader, healthcare management professionals must have a solid understanding of healthcare concepts. Depending on what career field they choose, they should know how their department impacts the organization’s bottom line. Areas that healthcare managers must have knowledge of include:
Patient care
Patient care is the focus of every healthcare provider, whether they are a single-physician office or a national hospital system. Even departments that don’t directly interact with patients, such as accounting, must understand the patient workflow, from scheduling to billing to reimbursements. Patient privacy, safety, and quality of care are often part of every department’s metrics.
Healthcare technology
Healthcare technology has expanded far beyond state-of-the-art medical devices. Technology such as artificial intelligence (AI) and patient electronic health records (EHRs) are now an everyday part of healthcare. AI is used in patient scheduling and diagnosing. EHRs are used across most of the industry. The data produced by healthcare technology is used to analyze operations and performance.
Healthcare regulations
The Health Information Portability and Accountability Act (HIPAA) governs patient health records and privacy. Medicare regulations govern how providers get reimbursed for care. According to the American Hospital Association, hospitals must comply with more than 600 separate regulations, and new rules are frequently adopted.
Healthcare revenue cycles
Understanding the revenue cycle of a hospital, physician’s office, nursing home, or other provider is essential to an effective healthcare finance career. All the steps of the revenue cycle must be integrated into the administrative operations of the healthcare provider. Data captured from the revenue cycle can help a facility better understand its operations. For example, too many billings that go to collections could indicate a problem at the patient registration step.
Physician practice management
Good financial management is essential to a thriving physician practice. A well-trained healthcare financial administrator will be knowledgeable about compliance with the Stark Law (an anti-kickback statute), financial reporting, and contract evaluation, among other best practices.
Managed care
Understanding managed care means understanding how healthcare insurance intersects with healthcare. It is crucial to how providers get paid. Effective healthcare finance managers will have a strong background in managed care and health insurance.
Financing and capital
Healthcare is a capital-intensive industry. Financial administrators must understand capital, debt, bond issues, and other financing issues to ensure their organization’s financial well-being. They may also be involved in making decisions regarding debt, capital projects, and other strategic initiatives.
Healthcare policy, strategy, and innovation
Healthcare is a dynamic industry, and healthcare policy is ever-changing. Effective management requires a mindset that is innovative and forward thinking. Examples of innovation in healthcare strategy and policy include:
The impact of COVID-19
The pandemic changed the way hospitals and doctors treat patients. Now, policies such as telemedicine have become part of the day-to-day operations of some providers. The pandemic also spurred innovations that were adopted almost immediately, rather than taking years to filter through the industry. The rapid development and deployment of the coronavirus vaccine is a case in point.
Price transparency and surprise billing
Hospital charges have typically been a source of great anxiety and confusion to most patients. Surprise billing, by which a patient finds out they’re responsible for thousands of dollars in hospital bills after a surgery or emergency room visit, has earned the hospital industry some black marks. Recent legislation is designed to foster price transparency and eliminate surprise billing.
Value-based care vs. fee-for-service
U.S. hospitals and other providers traditionally have been paid under a fee-for-service model. However, the industry is moving toward value-based care, which stresses preventive healthcare to improve patient outcomes and reduce costs. This move has changed the way providers are reimbursed for care. Understanding the new model is essential to making sure that providers get paid for their services.
Human resources
As the COVID-19 pandemic has shown, doctors and nurses are vulnerable to fatigue and stress due to overwork, which can lead to many bad outcomes, including a burned-out workforce. Properly managing staffing is essential to providing quality care to patients and maintaining a safe and rewarding workplace for employees. Human resources issues significant to the healthcare industry include:
Shortage of qualified health professionals
In the U.S. alone, employment in healthcare is expected to grow 15% from 2019 to 2029, according to the U.S. Bureau of Labor Statistics. Demand is rising due to an aging population, and because many healthcare professionals are retiring. A significant shortage of nurses is projected nationwide, for example, and many rural areas are experiencing physician shortages.
Scheduling
Scheduling nursing and other clinical staff is an art form. Administrators responsible for shift scheduling in physician practices, nursing homes, hospitals, and other facilities have a variety of software options to make the process more efficient.
Certification and training
Ensuring staff are trained and that all of their certifications and licensures are up-to-date is another essential administrative task. Expired certifications and licenses pose legal, regulatory, and quality risks. Other training, such as cybersecurity training, is increasingly the responsibility of healthcare administrators.
Creative thinking, communication, and problem-solving
High-level healthcare management careers place a premium on creative thinking and problem-solving. Many of the issues that face healthcare providers require innovation and creative strategies. Skills for a successful manager include:
Value creation
Preventive medicine, telemedicine, data analytics, and the use of AI and other technologies are changing the way healthcare is delivered. Managers and executives who understand these concepts are positioned to create new business models that meet the healthcare challenges of the future.
Communication
Negotiation and persuasive communication are an important part of a healthcare professional’s arsenal of tools. Managers and administrators must be able to present their ideas to the leadership team. Effective communication with patients and community outreach are essential to building trust and getting buy-in when introducing new care models, for example.
Data analytics and decision-making
Data analytics, blockchain, big data, and other digital concepts are expanding in influence in the healthcare sector. Managers and administrators must understand how data can be used to support decision-making and strategy.
Healthcare marketing
To be competitive, healthcare providers must market their services to patients, to their local communities, and even nationally or internationally. Healthcare marketers must create and deploy marketing campaigns that support their organization’s brand and mission while also building name recognition and trust in patients and potential patients. Healthcare marketing activities include:
Digital marketing
Digital marketing, including email, social media, and video, are ways to raise a provider’s profile. Digital marketing can be an effective part of an overall marketing strategy.
Thought leadership development
Highlighting physicians, nurses, and other providers as thought leaders can boost patient and community trust. For example, some hospitals make their healthcare experts available for news articles or features on current events in healthcare.
Medical services advertising
With a marketing strategy in place, healthcare marketers can use their channels — social media, video, newsletters, and other tools — to promote their medical services to potential patients.
Salaries and job outlook for healthcare management careers
The high demand for healthcare providers, especially nurses and doctors, is good news for professionals who are seeking a career in healthcare management. As mentioned above, employment across all healthcare occupations is expected to grow 15% between 2019 and 2029, according to the BLS. Additionally, the median wage for all healthcare occupations is significantly higher than the average median wage for all occupations.
Hospital CFO salary and outlook
The average annual salary for a hospital CFO was about $152,000 as of July 2021, according to ZipRecruiter. The number of jobs for financial managers in all industries is expected to rise 15% between 2019 and 2029, according to the BLS, indicating a solid demand for this profession.
Clinical informatics manager salary and job outlook
The median annual salary of clinical informatics managers was around $96,000 in June 2021, according to PayScale. At the highest experience level, the median salary was $130,000, per PayScale. Clinical informatics managers fall under the broader medical and health services manager group identified by the BLS. Demand for health services managers is expected to grow 32% between 2019 and 2029.
Hospital administrator salary and job outlook
The median annual salary of hospital administrators was around $87,000 in July 2021, according to PayScale. Salaries vary depending on factors such as experience, education, location, and organization; the top 10% of earners bring in about $150,000. As with other medical and health services managers, demand for hospital administrators is expected to grow at the rate of 32% between 2019 and 2029.
Nurse manager salary and job outlook
The median annual nurse manager salary was around $87,000 in July 2021, according to PayScale, with salaries in the top 10% rising to $118,000. Nurses are in high demand due to a shortage of professionals at all levels. Many nurses are retiring and nursing schools have not been able to train enough incoming nursing students to fill the need. Demand for advanced practice registered nurses is expected to grow 45% between 2019 and 2029, according to the BLS.

